
Human papillomavirus (HPV) is a group of common pathogens that can infect the skin and mucous membranes. The pathology is mainly diagnosed in patients between the ages of 20 and 30, as well as in children under 5 years of age. According to statistics, about 22 percent of the world's population are carriers of HPV. Many patients are affected by several strains at the same time.
More than 190 pathogen genotypes are currently known. They differ in DNA structure, course and possible complications. 30 pathogens can infect the epithelium of internal and external genital organs. It is worth noting that many HPV strains are characterized by pronounced carcinogenic activity. Therefore, the virus often causes life-threatening complications: malignant tumors of the vagina, vulva, anal tract, penis.
Causes of HPV
The only cause of infectionhuman papillomavirusis contact with the causative agent of the disease. However, certain factors significantly increase your chances of becoming infected. Right:
- Refusal to use barrier contraception. Only a male or female condom, as well as special latex wipes, can protect against infection.
- Frequent change of sexual partners. If you do not pay enough attention to your own safety, the risk of infection increases significantly.
- Early entry into sexual relations. Sexual relations during adolescence often lead to HPV infection due to an irresponsible attitude towards preventing the transmission of pathogens.
- Non-observance of hygiene rules. Insufficient self-care leads to the growth of pathogenic microflora on the skin and mucous membranes, which negatively affects susceptibility to the virus.
- Bad habits. Addictions significantly affect the body's immune defenses: alcohol abuse, smoking, taking psychoactive substances.
- Weakened immunity. The causes of the condition can be a lack of vitamins and minerals, chronic diseases and psycho-emotional overload.
- Long-term drug treatment. Hormonal drugs taken over a long period of time have a particularly pronounced effect.
- Traumatic injuries. Injuries to the mucous membrane and skin become a "gateway" for infection.
- Chronic stress. They also affect the patient's immune system and hormonal background.
- Gynecological interventions. Risk factors for HPV include miscarriages or miscarriages.
- Pregnancy. Often the disease first appears during pregnancy. Pregnancy is associated with increased stress on the body, which increases susceptibility to pathogenic flora.
Risks include certain diseases, such as uterine dysplasia. Regular preventive visits to the gynecologist and urologist help to significantly reduce the risk.
Symptoms

Of the total number of carriers of the causative agent, clinical manifestations of the papilloma virus are detected in only 5-10 percent of patients. The first symptoms may appear several months after infection or after several years. However, in this state the person poses a threat to others. It can infect other people by contact. Symptoms can be divided into subjective, which indirectly indicate pathology, and objective characteristic manifestations of HPV. Subjective symptoms include:
- Papules. These are single or multiple formations that protrude above the skin or resemble spots. They appear on the skin and mucous membranes of the urogenital area.
- Itchy skin. The patient often complains of itching in the genital area or other parts of the skin.
- Paresthesia. This is a sensitivity disorder in the affected area. The opposite manifestation often occurs - dyspareunia. In this case, every contact brings pain.
- Urinary dysfunction. When emptying the bladder, there is a feeling of burning, itching and pain. If the urethra is affected, urine output can be significantly more difficult.
- Cracks. Bleeding cracks appear on the skin and mucous membranes, which cause severe pain.
Such clinical manifestations may indicate various diseases of the genitourinary system. Objective symptoms of HPV allow an accurate diagnosis. Such signs include:
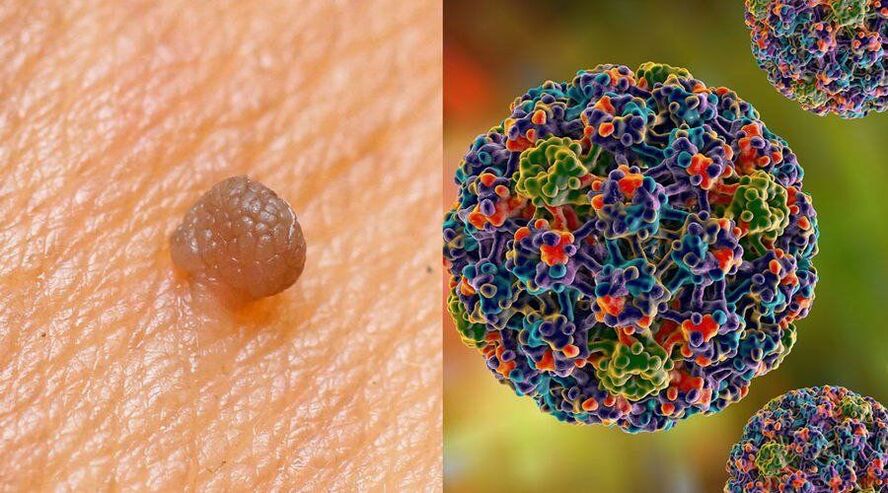
- Genital warts. This is an elevation above the surface of the skin, characterized by an elongated finger-like shape. Localized in the genital area. They differ in a specific pattern: colorful or in the form of a loop.
- Papular warts. They appear on the keratinized areas of the genitals. It can be straight or plain.
- A stain. The nature of the stains varies. There are bright red, brown with red shades, pink-red, white with gray.
- Bowen's disease. These are papules or spots characterized by a shiny or velvety surface. The shade varies from red to almost black.
- Giant warts. It is a small formation that gradually increases in size and merges into one.
- Respiratory papillomatosis. In this case, the formations are localized in the oral cavity, respiratory tract and lungs.
Also, HPV in women in the later stages can manifest as uterine cancer. In 2008, it was established that this particular virus is the cause of malignant tumors. Cervical cancer does not occur as an independent disease. The pathology is accompanied by heavy bleeding, pain in the abdomen and lower back, discomfort during intimacy, etc.
Transmission paths
Doctors and scientists still argue about the contagiousness of the human papillomavirus. Many experts believe that one contact without the use of barrier contraception with an asymptomatic carrier is enough for the probability of transmitting the pathogen to a healthy partner to reach 70 percent. Other doctors say that such risks are relevant only when they are in contact with papilloma carriers. Statistics show that with regular proximity, transmission of the virus to a healthy person occurs within a period of up to 6 months.
Infection can appear in different ways. How the papilloma virus is transmitted:
- Sexual transmission. The main way of infection is sexual contact. When using a condom, the risk is reduced to 10 percent. However, the pathogen can penetrate during other intimate manipulations, for example, during a kiss.
- From mother to baby. A newborn can be infected with HPV from the mother during passage through the reproductive tract. Typical outcomes of this situation are cases of laryngeal papilloma and anogenital warts.
- Contact and home route. The virus is also transmitted by ordinary household contacts. Most often it happens in common areas. The risk of infection is particularly high in bathrooms, saunas, gyms and swimming pools. Public toilets.
- Autoinfection. It is the transfer of the virus from the affected area to a healthy one, which occurs during shaving and hair removal.
Pathogenesis

Pathogenesis is significantly influenced by the key capability of HPV. This is the only virus that does not penetrate the blood, and therefore does not cause an inflammatory process. In a simplified form, the pathogenesis of human papillomavirus is as follows:
- Infection. The source of viral agents can be another person or objects in common use. The risk of transmission is significantly increased by microtraumas on the skin and mucous membranes: wounds, cuts, cracks, acne.
- Incubation period. Pathologies that develop as a result of HPV penetration into the body usually have a latent beginning. There is no exact duration of the incubation period for this disease. The phase lasts 1-3 months or reaches 2-3 years.
- Chronic presence Despite the absence of clinical manifestations, the disease is constantly progressing. A person becomes a source of viral agents for others.
- Visual manifestations on the skin. The result of the infection is the appearance of a benign or malignant formation at the point of entry of the virus.
In the initial phase, the pathogen affects the basal epithelial layer, mainly localizing on the mucous membranes of the genital organs, oral cavity and conjunctiva. The viral agent is capable of replicating exclusively within the basal epidermis without penetrating the bloodstream. Due to this feature, the body's immune system cannot fight the pathology to the greatest extent, but it works extremely limited.
The main cause of oncological pathologies on the background of HPV is the increased release of specific proteins that affect the process of cell division. First of all, the proteins responsible for blocking tumor changes, controlling the life cycle and protecting against replication in the presence of DNA damage are affected.
Classification
Due to the variety of strains, HPV types also differ significantly from each other. Many experts use several pathogen classifications at once. Therefore, depending on the clinical picture, all cases of HPV can be divided into asymptomatic and those with characteristic manifestations. There is a subclinical course in which periods of exacerbation are noted. Depending on the location, they differ:
- Skin. This type of human papillomavirus causes growths on the skin of an infected person.
- Anogenital. In this case, papillomas can be found mainly on the mucous membranes of the genital organs and in the anal area.
Often the main cause of discomfort for the patient is the external signs of HPV. When evaluating a pathogen, physicians focus more on the carcinogenicity of the strain. Right:
- Types of HPV that are not able to cause malignant tumors. These include strains 1-5, 10, 28 and 49.
- Types of pathogens with reduced oncogenic activity. They can cause cancer, but in extremely rare cases. Among such strains are 6, 7, 32, 40-44 and others.
- It is characterized by moderate oncogenicity. The proportion of affected cells that degenerate into cancer cells is quite high. The group includes strains 52-58, 30, 26 and others.
- Dangerous forms of human papillomavirus. It is these strains that predominantly provoke malignant tumor formations. This includes 16, 18, 64, 73 and others.
Diagnosis of human papilloma virus

Various diagnostic techniques help identify papillomas in men and women. Therefore, only molecular biological studies are effective for establishing a diagnosis in a patient with a latent form. The most common and well-known method is PCR. It is aimed at determining the genetic properties of the material taken from the patient. PCR helps to identify not only the fact of infection, but also the specific strain of HPV. Subclinical and clinical forms can be diagnosed by methods such as:
- Simple colposcopy. Papillomas, warts and spots can also be detected during a routine visual examination. Colposcopy refers to the examination of the vaginal opening using a special binocular device. The examination may be accompanied by the collection of biological material for research.
- Extended colposcopy. During the examination, additional tests are used. A test with 3% acetic acid, which causes the narrowing of unchanged blood vessels, is indicative. Additionally, an adrenaline test and a Chrobak test (if cancer is suspected) may be recommended.
- Cytological examination. To carry out the diagnostic procedure, you will need material from the epithelium or skin cells. The sample is used to determine the DNA of the virus, as well as to rule out cancerous tumors. Usually, cytology reveals only the most oncogenic types of viruses.
It is better to plan the collection of biomaterials for papilloma virus in women in the first half of the menstrual cycle, but not earlier than the fifth day. As a last resort, you can donate biological material later, if there are more than 5 days left until menstruation. You must not rinse your vagina before the procedure. It is worth excluding sexual intercourse two days before collection. A similar rule applies to intravaginal ultrasound and colposcopy.
When diagnosing HPV in men, material is collected from the urethra. It should have been at least two hours since your last urination. It is important to avoid intimacy for 48 hours before the test. Otherwise, the study may show false results.
Complications

Complications of pathology include excessive growth of warts and papillomas. In rare cases, purulent-septic processes occur against the background of damage to the formation. Typical consequences of infection with oncogenic strains are the following conditions:
- Anal cancer. 80 percent of cases of detection of this malignant tumor are associated with HPV infection. Also, negative factors that influence the occurrence of anal cancer are anal sex, smoking and hereditary predisposition. The disease may not manifest itself for a long time. Typical symptoms of the condition are rectal bleeding, itching and a foreign body sensation.
- Cancer of the vagina. 70 percent of patients with this diagnosis suffer from human papillomavirus. The condition usually occurs in women over the age of 40. Females over 70 are more susceptible to pathology. In the first stages, the symptoms can be confused with menstruation. In addition, pain in the pelvic area, constipation and tightness in the vagina occur.
- Cancer of the oral cavity and pharynx. A third of diagnoses are the result of HPV infection. The patient complains of pain when swallowing and eating food. In a calm state, there is a sensation of a foreign body in the larynx. In the later stages, general weakness, nausea and loss of abilities appear.
- Penile cancer. 50 percent of cases are caused by viral agents. This is a rare malignant tumor involving a tumor process localized in the male genital organ. Pathology is typical for men over 60 years old.
HPV treatment

There is currently no effective treatment for HPV. Therapeutic tactics for the papillomavirus can be built in two ways:
- Warnings about infections. Unfortunately, even the regular use of contraception and a careful approach to hygiene do not protect a person from infection. Of course, this significantly reduces the chances. However, most cases of transmission of the pathogen were recorded in persons during adolescence, at the age of 15-16 years. By the age of 25, the first symptoms already appear. For a pronounced effect, prevention must be carried out from an early age.
- Treatment of diseases caused by human papillomavirus. If the strain causes a malignant or benign formation, then therapy for the identified pathology is required. Papillomas are removed in cosmetic or medical offices. Cancerous tumors require complex multi-stage treatment depending on the stage.
Of course, there is good news. So, people with a normally functioning immune system can fight off HPV on their own within two years. Patients infected during adolescence become free of the viral agent by the age of 30. Unfortunately, those who have recovered do not gain lifelong immunity.
Forecast
A significant part of the strains is characterized by low or moderate oncogenicity. Only certain types of viruses are associated with an increased risk of developing cancer. These statistics allow us to give many patients a positive prognosis regarding HPV. Early detection of malignant tumors significantly increases the chances of recovery.
The discovery of a virus that can cause cell damage has three potential outcomes:
- The virus exists, but it has not yet changed the cellular structure. In this situation, the patient will be classified as a risk group. If a cancerous type is found, regular follow-up by a gynecologist or urologist is necessary. In addition, you should undergo periodic tests.
- Changes in CIN-1 cells are detected in the early stages. For the most part, this condition also does not require medical intervention. Typically, a control examination is carried out once a year to ensure that the pathology does not progress.
- Marked changes in CIN-1 were noted. To rule out dangerous conditions, a biopsy is required. The study will determine whether the formation is of an oncological nature.
Prevention

You can prevent HPV infection by following key prevention rules. Important:
- Visit doctors on time. Women are recommended to schedule visits to the gynecologist 1-2 times a year. Men should see a urologist on a similar schedule. If you have risk factors (frequent changes of sexual partners, refusal of contraception), you should visit the doctor more often.
- Reduce visits to public places - swimming pools, saunas, bathrooms. If this is not possible, then it is important to use your own towel, not to take other people's razors and not to sit on the surface of your naked body.
- Use contraception. Only barrier methods are effective. The use of oral contraceptives does not affect the strains.
- Reject bad habits. Quitting smoking and moderate alcohol consumption will have a moderate effect on the body's condition.
- Increase the body's immune defenses. Proper nutrition, regular physical activity, following a daily routine, exercise have a beneficial effect.
- Avoid stress. Psychoemotional overload can negatively affect the immune system, so it is better to exclude them.
It is important to test yourself periodically. If there were situations in which an infection could have occurred, then it is better to do an HPV test. There are also people in danger. so:
- patients aged 21-30 should have a PAP test at least once every five years (preferably using liquid cytology);
- people aged 30 to 65 must undergo Pap testing for HPV every three years with mandatory PCR for oncogenic forms (16 and 18).
HPV in pregnant women

Human papilloma in women, as a rule, does not pose special risks for childbearing. Anogenital warts deserve special attention. They are localized not only on the outer lips, but also in the vagina. In some cases, they are accompanied by a bacterial component. Anogenital warts significantly increase the risk of infection of the baby during childbirth. This is loaded:
- Recurrent juvenile laryngeal papillomatosis. A similar situation is caused by four strains of HPV. Usually, the pathology is due to anogenital warts or HPV of the genital type.
- Increased risk of developing cancer in adulthood. Infection with the virus at such an early age significantly affects susceptibility to cancer in the future.
Let's take a closer look at laryngeal papillomatosis. Currently, it is not completely known at what point the viral agent is transmitted. Infection can occur through the placental barrier or directly at the time of the child's birth. The first symptoms of pathology are hoarseness. In severe cases, the baby's voice disappears completely and breathing difficulties appear.
The disease is capable of rapid progression. A little later, the patient develops a cough and constant shortness of breath. In the background of HPV, the child can experience asphyxia caused by the blockage of the respiratory tract. Most often this happens when there are papillomas on thin legs.
A special medical device called a laryngoscope is used to diagnose the disease. It can be replaced by a bronchoscope. The devices allow us to identify the main sign of pathology - the growth of the larynx (condyloma). Surgical treatment is usually recommended for the child. Condylomas are removed by destruction (freezing) or excision. However, the aggressive nature of the disease often leads to relapse.
A future mother infected with HPV with a high degree of oncogenicity should inform the obstetrician at the prenatal clinic. In this case, doctors will take all measures to ensure that the virus does not affect the child's health.


















